deciphering the discipline
A regular column offering the student perspective of the next generation of ceramic and glass scientists, organized by the ACerS President’s Council of Student Advisors.

Sadaf Batool
Guest columnist
Challenges in fabricating 3D-printed scaffolds for bone tissue regeneration
Though bone has a remarkable innate ability to heal itself after damage and illness, external support is required for bone repair to treat large defects and infections. This external support can take the form of structures that hold the damaged parts in place and/or bioactive materials that help stimulate regeneration.
Bone autografts and allografts are currently the gold-standard for treating bone defects. However, both these methods have several limitations, such as immune system rejections, morbidity issues, and transfer of infectious diseases. On the other hand, metals, wood, polymers, and calcium phosphate-based materials have been used for centuries as external support materials. But these materials suffer from challenges involving biocompatibility, immune system rejection, poor mechanical strength, and stress shielding effect, respectively.
To get optimal benefits from scaffolding, scaffolds should emulate the innate hierarchical structure of bone.1 Specifically, scaffolds should have an interconnected porous structure for active transport of cells and nutrients to the growing bone, as well as adequate mechanical strength to support the damaged bone. An ideal scaffold would also be biocompatible, osteoinductive, biodegradable, and bioresorbable.
All these requirements cannot be fulfilled using conventional fabricating methods. But recently, additive manufacturing techniques have allowed scaffolds to be fabricated with these desired properties. Additionally, these techniques provide flexibility in geometry design so defects of any shape and size can be treated.2
Typically, 3D-printed scaffolds are created using an organic–inorganic hybrid structure that features synthetic and biopolymers matrices reinforced with metallic and/or bioceramic nano-particles. This hybrid approach faces some challenges, however.
For one, synthetic polymers have poor biocompatibility and are generally nonbiodegradable, while biopolymers have poor mechanical strength. The biopolymer limitation can be overcome by crosslinking the polymers in such a way as to form a complex network that maintains its structure in vivo for a regeneration period. However, once this structure is achieved, it becomes difficult for the metallic/bioceramic nanoparticles to interact well with the polymeric chains, which leads to issues with the flowability and stability of the ink during printing.
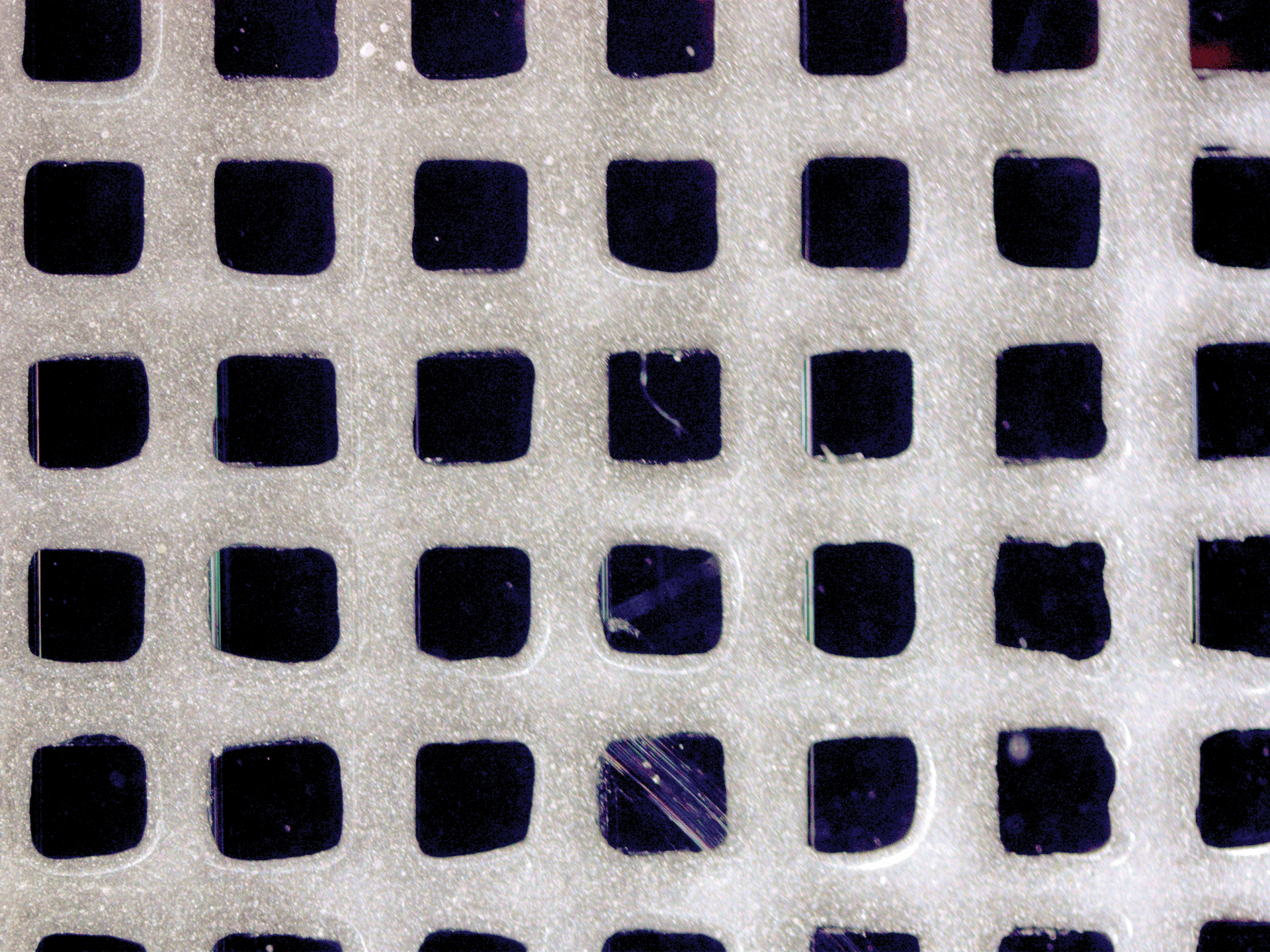
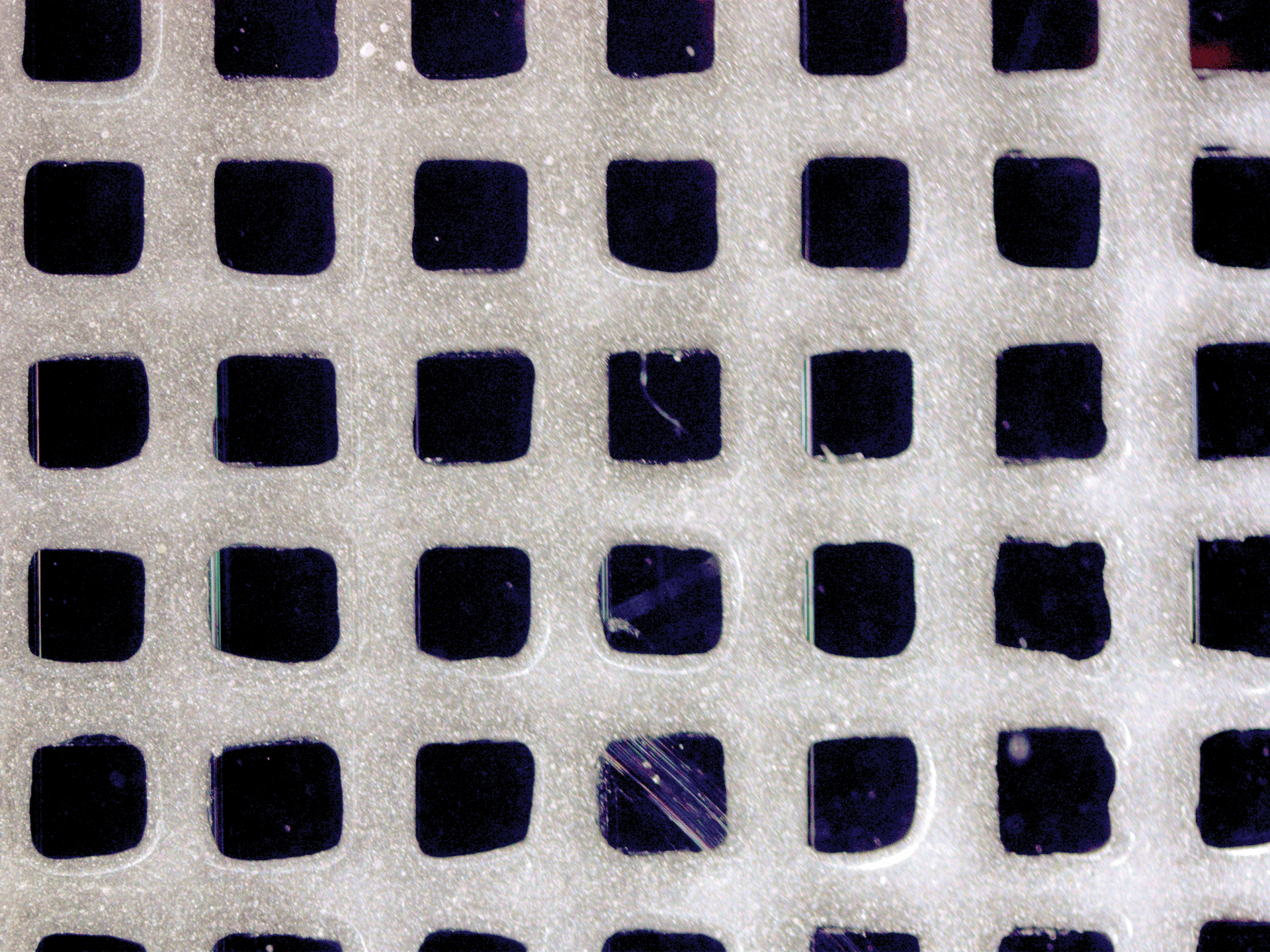
Figure 1. Close-up image of the calcium magnesium phosphate scaffold, created using gelatin and a ceramic bioink.
Credit: Sadaf Batool
This issue of nanoparticle aggregation can be overcome in several ways. For example, the nanoparticles’ surfaces can be functionalized to interact with the polymer chains via noncovalent linkages. Or, the mixture could be sonicated for an extended period so the nanoparticles have time to settle themselves in the empty interstitial space between polymers.
After successful ink formation, process parameters must be carefully considered to ensure the ink flows and cures as desired. As crosslinking is done after printing, the printed scaffold needs to maintain its structural integrity until that process takes place.3 To maintain ink stability, printer head pressure and temperature must be held steady during printing. The bed temperature is also critical to maintaining ink stability.
I have personal experience with creating bioinks, as my Ph.D. research is focused on creating ceramic composites for bone tissue regeneration. So far, I have created bioinks based on gelatin and calcium magnesium phosphate, which I used to print a grid structure of four layers (Figure 1).
The bioink was prepared by the oxidative polymerization method, and the conditions that allowed for each layer to be printed with intact structure and uniform porosity were optimized after hundreds of failed reactions. The printed structure was stable and showed excellent bioactivity and cell proliferation results.
Some analyses of my printed structures are ongoing. In future experiments, I hope to increase the number of layers so that the scaffold can be used for commercial applications.
About the author:
Sadaf Batool is a Ph.D. candidate in nanoscience and engineering at the National University of Sciences and Technology, Islamabad, Pakistan. Her doctoral dissertation is based on the synthesis and fabrication of calcium magnesium phosphate-based composites for bone tissue regeneration. She conducted part of her doctoral dissertation work at the Institute of Biomaterials at Friedrich Alexander University Erlangen-Nuremberg, Germany, with funding from the Higher Education Commission of Pakistan. She likes to do photography, cooking, and traveling in her free time.